
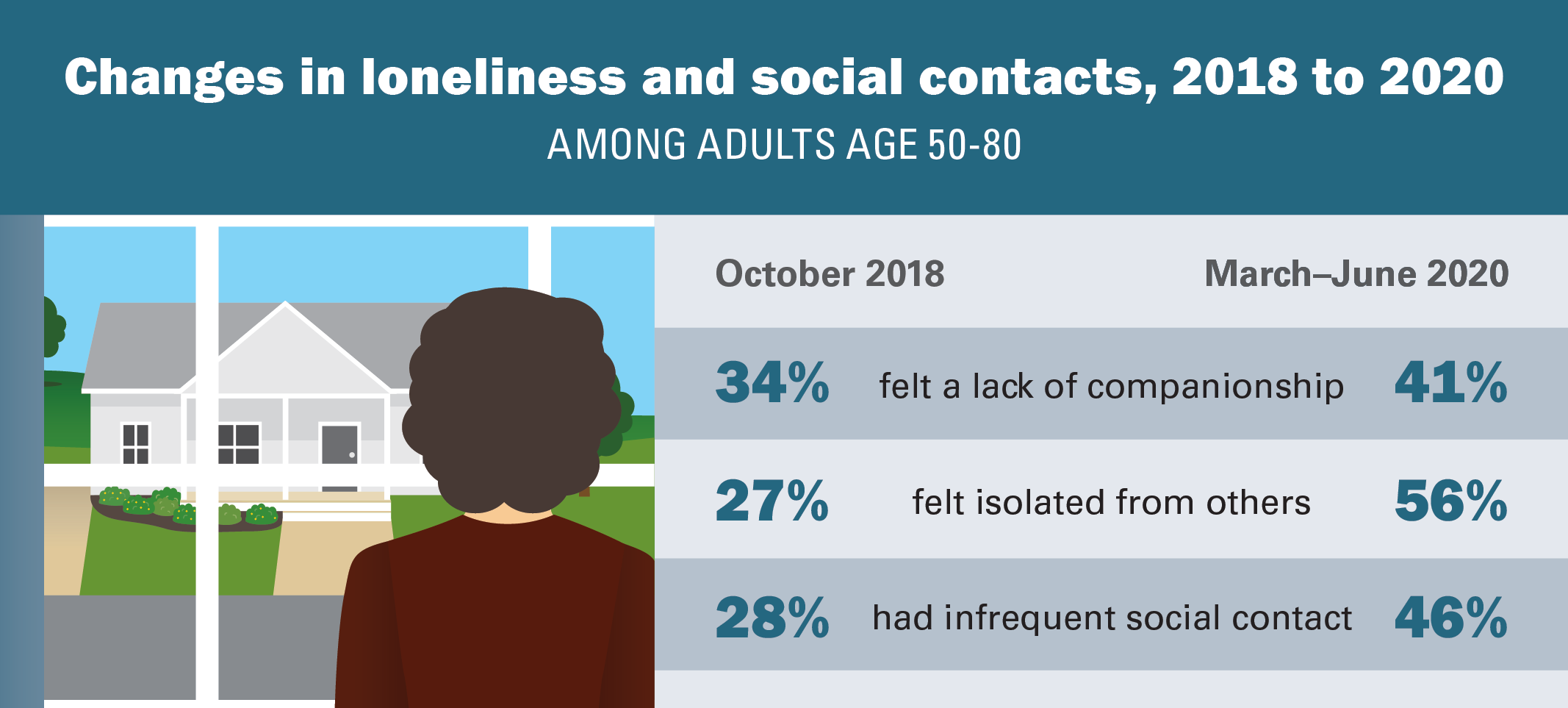
The University of Michigan National Poll on Healthy Aging (NPHA) asked a national sample of U.S. adults age 50–80 about lack of companionship and isolation (loneliness), social interactions, and health behaviors in June 2020. This was a follow-up to a similar NPHA survey conducted in October 2018 among a different national sample. The comparisons that follow show a substantial increase in loneliness among older adults from before the COVID-19 pandemic to the period March–June 2020.
Lack of companionship
Two in five adults age 50–80 (41%) reported feeling a lack of companionship (32% some of the time, 9% often) during the early months of the pandemic, compared to 34% (26% some of the time, 8% often) in 2018. In June 2020, one in three older adults (35%) said they felt less companionship compared to before March 2020, 12% felt more, and 53% felt the same amount of companionship.
Social isolation
In June 2020, more than half of older adults (56%) reported feeling isolated from others (43% some of the time, 13% often) compared to 27% (22% some of the time, 5% often) in 2018. When comparing their feelings in June 2020 to before the pandemic, about half of adults age 50–80 (48%) felt more isolated, 8% felt less isolated, and 44% reported feeling the same level of isolation. Nearly half of older adults (46%) in June 2020 reported infrequent social contact (once a week or less) with family, friends, or neighbors from outside the home, compared to 28% in 2018.
Who experiences loneliness
Feeling a lack of companionship some of the time or often during the first three months of the pandemic was more common among women (47% vs. 35% of men), people who lived alone (50% vs. 39% who lived with others), and those who were unemployed, disabled, or not working (52% vs. 39% of those employed or retired). Others more likely to report a lack of companionship included those from households with annual incomes less than $60,000 (46% vs. 38% of those with higher incomes) and caregivers (48% vs. 40% of non-caregivers). In addition, feeling a lack of companionship was more common for those who reported fair or poor physical health (52% vs. 39% of those reporting excellent, very good, or good physical health) or fair or poor mental health (68% vs. 39% of those reporting excellent, very good, or good physical health), and more common for those reporting more symptoms of depression (84% vs. 36% among those with fewer symptoms).
There were fewer notable differences among respondents in feelings of isolation from March–June 2020. Women were more likely to report feeling isolated (61% vs. 50% of men), as were people in fair or poor mental health (72% vs. 55% of those reporting excellent, very good, or good mental health), and people reporting more symptoms of depression (89% vs. 52% among those with fewer symptoms).
Infrequent social contact (once a week or less) with people outside of the household was more common among individuals age 50–64 (49% vs. 42% of those 65–80), men (52% vs. 41% of women), and those who lived with others (48% vs. 41% of those living alone). Infrequent social contact was also more common for those reporting fair or poor physical health (53% vs. 45% of those with better physical health), fair or poor mental health (58% vs. 45% of those with better mental health), and individuals with more depressive symptoms (64% vs. 44% of those with fewer symptoms).
Social interactions
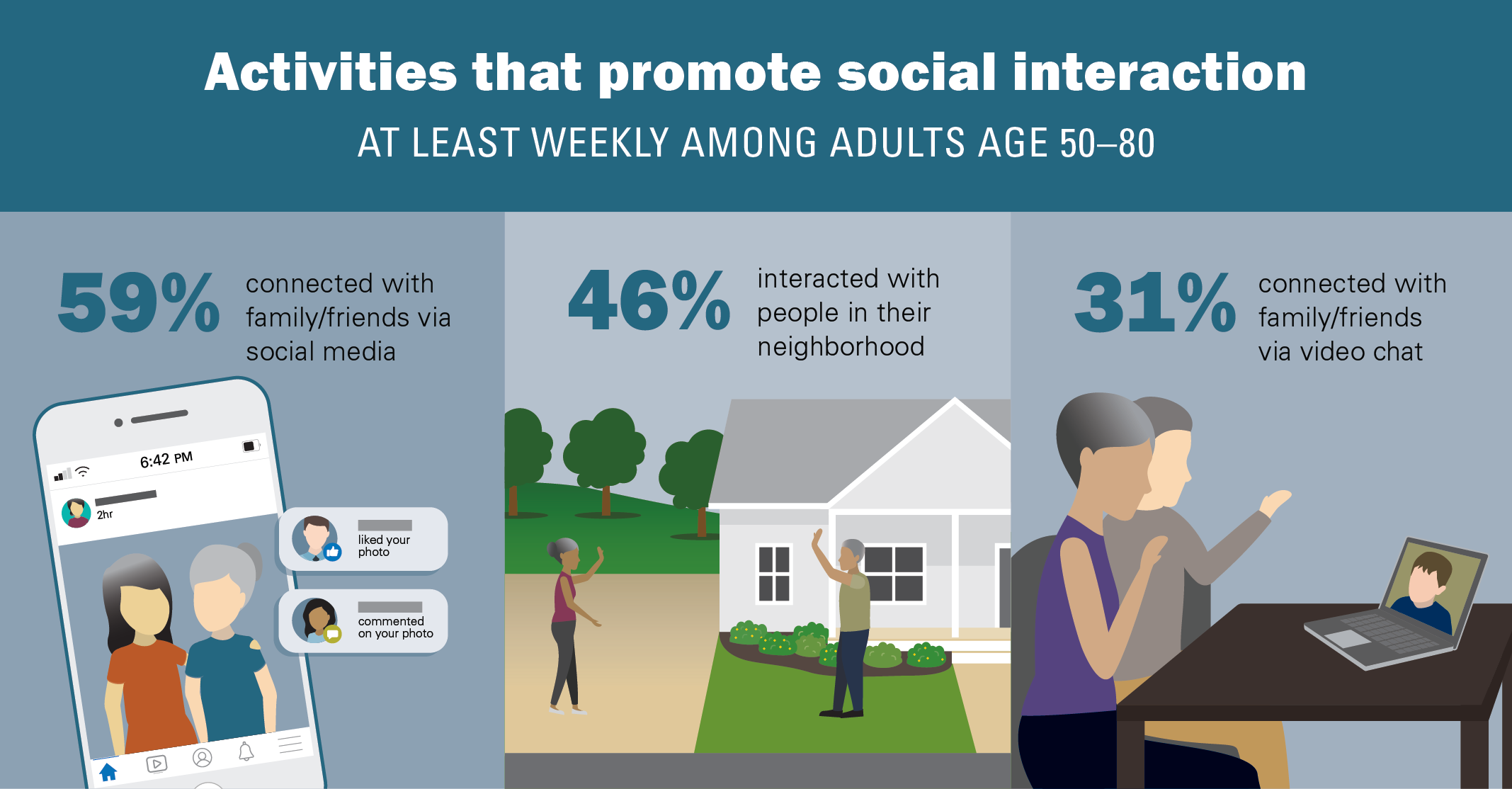
From March–June 2020, many older adults reported connecting with family or friends outside their home using social media (70%) and video chat (57%). Three in five (59%) used social media and 31% used video chat once a week or more. Yet adults age 50–80 who used social media were more likely to report feeling isolated than those who did not use social media (58% vs. 51%). There were no differences in feelings of companionship and isolation among those who used video chat compared to those who did not.
Nearly half of adults age 50–80 (46%) said they interacted with people in their neighborhood at least a few times per week, and three in four (75%) reported spending time outdoors or interacting with nature at least weekly from March–June 2020. Individuals who interacted with people in their neighborhood or spent time outdoors at least a few times per week were less likely to report feeling a lack of companionship or feeling isolated.
One in eight older adults (13%) said they had arguments with family or friends at least once a week from March–June 2020. Those who had arguments with family or friends at least once a week were more likely to feel a lack of companionship and feel isolated than those who had arguments less often or not at all.
Health behaviors
In 2018 and 2020, most older adults indicated they engaged in healthy behaviors several times a week. Four out of five reported getting enough sleep (80% in 2018 vs. 81% in 2020) and eating a healthy diet (80% in 2018 and 2020), and in both surveys, 62% said they exercised at least several times per week. In both survey years, people who regularly engaged in healthy behaviors were generally less likely to experience loneliness compared to those who did not.
Implications
The results of this poll suggest that the COVID-19 pandemic has had a substantial impact on feelings of loneliness (lack of companionship and isolation) and social connections among older adults. A greater proportion of adults age 50–80 felt a lack of companionship, felt socially isolated, and had infrequent contact with others from outside their home during the early months of the pandemic than in 2018 when those numbers were already worrisomely high.
Studies show that chronic loneliness can adversely affect memory, mental and physical health, and longevity. This poll found that loneliness and limited social contact during the pandemic were strongly associated with depressive symptoms and overall mental health among older adults. In addition, these results suggest that those who engage in healthy behaviors less frequently experience more loneliness than those who do things like get regular exercise and enough sleep.
It is important to recognize the pandemic’s impacts on the overall well-being of older adults and identify opportunities to mitigate them. The increases in loneliness and infrequent social contact may be at least partially explained by the important public health strategies used to reduce the spread of COVID-19 (e.g., stay-at-home orders). Yet even during these challenging times, increased efforts should be made to identify older adults at higher risk of feeling lonely, isolated, or socially disconnected from others, including those living alone and those with fair or poor mental and/or physical health.
These results suggest that the use of video chat and social media, while helpful for some, may not buffer feelings of loneliness for many older adults. On the other hand, those who interacted with others in their neighborhood and/or with nature experienced less loneliness. While personal interactions and social activities may look different during the COVID-19 pandemic (e.g., physically distanced, outdoors, or online), providing safe opportunities for regular and meaningful interaction with others and with nature is important to reduce loneliness and maintain social connections.
As the COVID-19 pandemic continues, it is critical for policymakers, clinicians, and family members to address feelings of loneliness among older adults to mitigate their effects on mental and physical health.
Data Source and Methods
This National Poll on Healthy Aging report presents findings from a nationally representative household survey conducted exclusively by Ipsos Public Affairs, LLC (“Ipsos”) for the University of Michigan’s Institute for Healthcare Policy and Innovation. National Poll on Healthy Aging surveys are conducted by recruiting from Ipsos KnowledgePanel®, the largest national, probability-based panel in the U.S.
This survey module was administered online in June 2020 to a randomly selected, stratified group of older adults age 50–80 (n=2,074). The sample was subsequently weighted to reflect population figures from the U.S. Census Bureau.
The completion rate was 78% among panel members contacted to participate. The margin of error is ±1 to 2 percentage points for questions asked of the full sample and higher among subgroups.
Findings from the National Poll on Healthy Aging do not represent the opinions of the University of Michigan. The University of Michigan reserves all rights over this material.
Citation
Piette J, Solway E, Singer D, Kirch M, Kullgren J, Malani P. Loneliness Among Older Adults Before and During the COVID-19 Pandemic. University of Michigan National Poll on Healthy Aging. September 2020. Available at: http://hdl.handle.net/2027.42/162549